Jump to: What’s the personal fat threshold? | What’s your personal fat threshold | The DiRECT trial: type 2 diabetes remission | Energy storage and digestion: fat | Energy storage and digestion: carbohydrates | Take home message
Welcome to part one of a four-part series on the personal fat threshold and type 2 development.
The four articles in this series will take you on a journey from understanding the complex management of energy in the human body to insulin resistance and, eventually, how it leads to the development of type 2 diabetes.
In this article, we’ll outline the personal fat threshold, how you can measure what your personal fat threshold is, and help you develop a deeper understanding of how the body regulates the energy we get from food.
The four articles are:
- What’s your personal fat threshold?
- Insulin and the personal fat threshold
- Insulin resistance and the personal fat threshold
- How to improve insulin resistance
Medication-assisted weight loss with a future focus
Start with Wegovy or Mounjaro, transition to habit-based health with our support

What’s the personal fat threshold?
Type 2 diabetes is a complicated disease with many theories about its development. One of those theories is the personal fat threshold hypothesis, which states that:
- Everyone has a limit on how much fat they store within the fat cells beneath the skin, which we call subcutaneous fat.
- Once this limit is reached, the body has to store the fat somewhere else, so it starts to build up in and around our internal organs, such as the liver and the pancreas. We call this visceral fat.
- When this fat builds up over time, it can negatively affect the liver and pancreas’s ability to manage blood sugar levels. This excess visceral fat build-up, coupled with increased insulin resistance, leads to the onset of type 2 diabetes and elevated blood sugar levels.
This theory helps explain why slim people can develop type 2 diabetes and people living with obesity.
We all likely have our personal fat threshold, and when we go beyond that – our body can no longer manage carbohydrates and fat effectively, and we can develop type 2 diabetes.
What’s your personal fat threshold?
Currently, there’s no way of accurately measuring your personal fat threshold. It’s also not something that currently has a number as a guide on the diagnosis.
However, from a practical perspective, we can define your personal fat threshold as the tipping at which your body starts to store more fat in and around your internal organs.
While not perfect, there are three ways we can measure this:
1) Waist circumference
This estimates how much visceral fat you have stored in and around your internal organs. You may be beyond your personal fat threshold if it’s too high.
In males, anything above 94cm (37in) is considered ‘high risk’. For women, it’s anything above 80cm (31.5in).
One thing to remember is that some people will have wide waists because they do strength training and have a lot of muscle; this doesn’t infer the same risk as a high waist circumference due to excess fat.
2) Waist-to-hip ratio
Similar to waist circumference, this indicates how much visceral fat you have. It’s calculated by dividing your waist circumference by your hip circumference.
A ratio of 0.95 or lower is considered healthy and low-risk in males. In females, it’s 0.80 or lower. As the level increases beyond these scores, your risk of developing chronic diseases like type 2 diabetes increases.
Again, the exception is in individuals with high muscle mass levels.
3) Liver fat
You won’t be able to walk into your GP practice and get your liver fat measured, unfortunately. This would require a scan at a hospital or research facility.
However, your GP will likely do regular liver function tests (LFTs), which can be measured in your blood.
While these won’t be able to give you an accurate measure of your liver fat levels, they can indicate whether you might have excess liver fat as the function of your liver will become more abnormal as the level of fat in your liver increases.
At Second Nature, we’ve been partnered with the NHS since 2017, providing support for individuals living with type 2 diabetes and pre-diabetes.
In our first pilot study with NHS Portsmouth CCG, 40% of individuals reduced their blood sugar levels to the normal range, and people lost over 9% of their body weight on average.
If you’re currently living with type 2 diabetes and would like to join the Second Nature programme to see if you can lower your blood sugar levels, improve your health, and reduce your reliance on medications, you have two options:
- Speak to your GP to see whether Second Nature is available in your area and whether they can refer you to the programme.
- Click here to take our health quiz and join over 150,000 others who’ve improved their lifestyle with Second Nature.
Otherwise, keep reading as we dive deeper into the science behind the personal fat threshold.
1) The DiRECT trial: type 2 diabetes remission
Our liver and pancreas regulate our body’s weight and health. In individuals with type 2 diabetes, we see high levels of fat stored within these vital organs. We call this visceral fat.
This excess visceral fat affects how well the liver and pancreas can function. One of the side effects of these organs being unable to function correctly is an increase in the amount of sugar in the bloodstream, which we use to diagnose type 2 diabetes.
We introduced Professor Roy Taylor’s work in the DiRECT study in our guide on diabetes remission. As a quick recap, the study split 298 individuals living with type 2 diabetes into two groups.
The first group (known as the control) were to continue standard treatment with their GP. In contrast, the second group (known as the intervention) were given liquid meal replacements that totalled 800 calories a day for 12-20 weeks, with the gradual reintroduction of whole foods for 2-8 weeks.
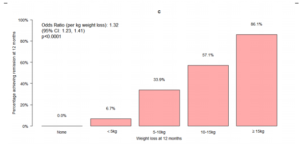
The study demonstrated that many people can put their type 2 diabetes into remission, with over 46% of individuals in the treatment group achieving an HbA1c below 48 mmol/mol after 6-months (the diagnostic threshold for type 2 diabetes).
For overweight individuals, losing more than 10% of their body weight can increase their chances of remission.
However, weight loss is only part of the story. We know that many individuals can develop type 2 diabetes even within the healthy weight range.
The role of visceral fat
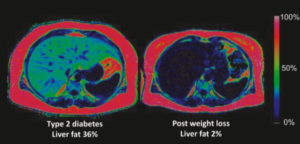
The DiRECT study also reported significant reductions in pancreatic and liver fat in participants who achieved remission, regardless of the total amount of weight they lost. This indicates that the fat stored within these organs plays a significant role in developing type 2 diabetes.
Illustrating this, below is an image of a participant’s liver in the trial. The image on the left shows the volume of liver fat at the start of the intervention (36%), and on the right, the volume of fat at the end of the trial (2%) when remission was achieved.
Our growing understanding of the role of the liver and visceral fat has supported the development of the personal fat threshold hypothesis.
This hypothesis states that everyone has a limit to the amount of fat they can store in the fat cells underneath the skin, which we call subcutaneous fat. Collectively, this is also known as our adipose tissue.
When this limit is reached, your body will start to store the fat within your vital organs (including the pancreas and liver).
This transition from fat storage under the skin to the internal organs could give us a greater understanding of how type 2 diabetes develops and how to provide more individualised support for people living with this condition, regardless of their BMI.
But before we discuss the mechanisms of the personal fat threshold in more detail, it’s essential to understand how the body stores and regulates energy. This will be the focus of the rest of this article.
Key points:
- Type 2 diabetes has many proposed theories as to how it develops
- Although it’s typically associated with obesity, the liver and the pancreas play critical roles in regulating our weight and blood sugar levels.
- Consistent in all theories, you typically see high levels of fat stored within the liver and the pancreas.
- To achieve diabetes remission, liver and pancreatic fat reduction are needed, no matter how much overall weight loss is achieved.
- The ‘personal fat threshold’ hypothesis states that we all have an individual limit of how much subcutaneous fat we can store in our bodies.
- When this limit is reached, our body will start storing fat in our internal organs as visceral fat, which leads to type 2 diabetes.
2) Energy storage and digestion: fat
Our body’s primary fat storage site is our adipose tissue. Adipose tissue is mainly found beneath the skin in the form of subcutaneous fat. It’s our most abundant source of energy: even a lean adult male will have around 50-70,000 calories of fat stored in their adipose tissue.
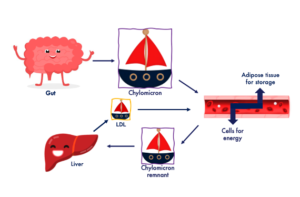
When you eat a meal containing fat, this fat will travel through the stomach to the gut. From here, the fat is moved into small transport ‘boats’ that carry the fat around the blood. We call these chylomicrons (pronounced ky-low-my-crons).
Chylomicrons are like boats as they transport fat (the cargo) around the body to the cells that need it. Depending on the requirements of each cell in the body, the fat will either be used for energy straight away or stored in the adipose tissue for later.
When the chylomicron has delivered most of its cargo to the cells and adipose tissue, it will become a smaller boat, which we call a ‘remnant’, with small amounts of fat remaining inside.
The smaller boat will then travel to the liver to be recycled. The liver will either store the leftover fat or send it out in other boats similar to chylomicrons known as low-density lipoproteins, or LDL.
LDLs perform a similar job as the chylomicrons, delivering fat around the body to either be used for energy or stored in the cells for later use.
Imagine the gut to be the port, the chylomicrons the boat, the fat the passengers, and the liver the shipyard. You can see this presented in the image below:
There will be a higher number of boats in your bloodstream in the hours after a meal.
The primary role of this system is to ensure that fat doesn’t remain in the blood (as this can damage cells) and that it’s either delivered to cells that require it for energy, such as the heart and muscles, or stored in our adipose tissue (our fat cells).
Having consistently high levels of fat in your bloodstream is a sign that this system isn’t working as well as it should and that your body is struggling to regulate fat effectively.
Key points:
- Fat is stored within our adipose tissue, predominantly found in subcutaneous fat beneath the skin.
- When you consume fat in a meal, it’s carried around the body in molecules known as chylomicrons.
- Chylomicrons act as boats, delivering the fat to the cells around the body to either be used for energy or stored for later use.
- Chylomicrons are then returned to the liver to be ‘recycled’ with any remaining fat stored in the liver or sent out in other boats known as low-density-lipoproteins.
- Low-density-lipoproteins will perform a similar job to chylomicrons.
- The primary role of this system is to keep levels of fat in the bloodstream low and provide the body with a vital energy source.
3) Energy storage and digestion: carbohydrates
When you eat carbohydrates in a meal, they’re transported through the stomach and into the gut, where they’re broken down into simple sugars such as glucose.
Glucose is then released into the bloodstream, which causes a rise in your blood glucose (sugar) levels.
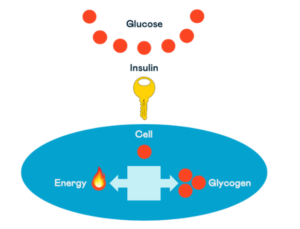
Your pancreas will respond to the rise in blood glucose by releasing the hormone to transport the glucose into the muscles and other cells of the body to be used for energy. We call this hormone insulin.
Insulin acts like a key; it opens the doors to the cells in your muscles to allow glucose to enter.
Once inside the cells, the glucose will either be used for energy or, if it’s moved into muscles, it can also be stored for later use. The storage form of glucose is called glycogen.
The body can store around 1500 calories of glycogen in the muscles or around 400 calories in the liver.
Insulin also plays a vital role in this process. We mentioned earlier that fat travels around the body in boats called chylomicrons, and depending on what the cell needs, fat will either be stored in the adipose tissue or used for energy.
To ensure that our cells aren’t ‘overloaded’ with fat and glucose simultaneously (think of an overflowing fuel tank), insulin tells the body to store the fat straight away in the adipose tissue rather than using it for energy.
This means the body will use this glucose for energy when glucose is higher in the blood after we eat a carbohydrate-rich meal. This meal’s fat will be stored in our fat cells rather than burnt for energy.
The reason your body does this is because of the limited amount of storage you have for glucose. As we only have around 2000 calories available to store excess glucose but a seemingly endless amount of fat cells to store fat, it’s easier for the body to burn the glucose and ‘spare’ the fat.
In parts two and three of this series, we explain how the energy systems described above become dysfunctional and lead to you going beyond your personal fat threshold.
Key points:
- All carbohydrates are broken down into simple sugars, such as glucose, and released into the bloodstream.
- Your pancreas reacts to higher blood glucose levels by releasing the hormone insulin.
- Insulin acts like a key, unlocking the door into the cells, which allows glucose to be used for energy or stored as glycogen.
- Your body has a limited capacity for storing glycogen, around 1500 calories in the muscles and 400 calories in the liver.
- Insulin also protects the cells from becoming ‘overloaded’ with energy by telling the body to store fat and use glucose as the primary fuel when we eat more carbohydrates.
Take home message
Type 2 diabetes is a complex condition, and there are multiple theories about how it develops. However, all theories agree that increased fat stored in the liver and pancreas plays a role.
The ‘personal fat threshold’ hypothesis states that every individual will have a level at which they can no longer store subcutaneous fat in the adipose tissue (the fat under the skin).
At this point, fat storage in the liver and pancreas will increase, and type 2 diabetes will develop or worsen.
Knowing how the body regulates and stores energy is essential to help us understand the potential mechanisms determining an individual’s personal fat threshold.
Our body regulates and stores fat and carbohydrates through different systems. However, insulin plays a vital role in the regulation of both.
Click here to read our next article in this series.


