Jump to: What’s insulin resistance? | Adipose tissue growth | Insulin resistance and the adipose tissue | Can you increase your personal fat threshold? | Take home message
Welcome to part three in our series on the personal fat threshold and type 2 diabetes. In parts one and two of this series, we’ve discussed:
- The personal fat threshold hypothesis.
- The body’s essential energy systems regulating fat and carbohydrates and how that will influence our personal fat threshold.
- How insulin is involved in the regulation of fat and carbohydrates.
In this article, we’ll focus on the role of insulin resistance, its impact on our adipose tissue (fat cells), and how this has a potential role in mediating our personal fat threshold.
Medication-assisted weight loss with a future focus
Start with Wegovy or Mounjaro, transition to habit-based health with our support

What’s insulin resistance?
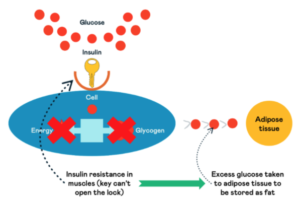
When regulating carbohydrates (glucose) in the body, insulin acts as a key. Unlocking the doors of the body’s cells allows glucose to enter.
Many body parts, such as the muscles, liver, and fat cells (adipose tissue), have these doors on them; we call these insulin receptors.
In insulin resistance, these doors become more difficult to unlock, and the body tries to send out more keys (insulin) to unlock them and allow glucose to enter. This can happen across the body, including our muscles and adipose tissue.
When this gets worse over time, the energy struggling to get through the doors of the cells remains in the bloodstream, where the body doesn’t want it. Insulin then decides to try and store it within our internal organs instead as visceral fat as a last resort.
This process is a crucial mechanism explaining how insulin resistance and high insulin levels can play a role in determining your personal fat threshold.
The body’s ability to store fat underneath the skin in adipose tissue protects the body from harm. As a reminder, this process ensures that:
- Excess energy doesn’t build up in the cells
- Excess energy doesn’t build up in the bloodstream
- Fat isn’t stored within the internal organs
The critical point is number three. This can be seen as the tipping point when fat storage increases in our internal organs and chronic diseases such as type 2 diabetes start to develop or accelerate.
At Second Nature, you’re supported by registered dietitians or nutritionists who are experts in treating type 2 diabetes through an improved lifestyle.
If you’re currently living with type 2 diabetes and would like to join the Second Nature programme to see if you can lower your blood sugar levels, improve your health, and reduce your reliance on medications, you have two options:
- Speak to your GP to see whether Second Nature is available in your area and whether they can refer you to the programme.
- Click here to take our health quiz and join over 150,000 people who’ve improved their health with Second Nature.
Otherwise, keep reading. This article will explore how the adipose tissue is key to identifying where your ‘tipping point’ of your personal fat threshold will be and how insulin, specifically insulin resistance, influences this process.
1) Adipose tissue growth
Adipose tissue can store excess fat by either increasing the size of existing fat cells (hypertrophy) or increasing the number of new cells from dormant cells we call pre-adipocytes (hyperplasia).
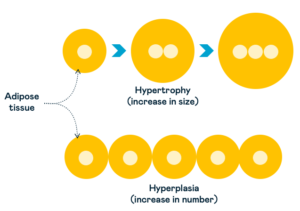
Research has shown that people who gain weight by increasing their fat cell number (hyperplasia) compared to increasing their cell size (hypertrophy) are less likely to develop insulin resistance and chronic diseases such as type 2 diabetes.
Storing excess fat by increasing the number of fat cells causes less harm to the body than increasing the size of existing ones. It may also mean you have a more significant personal fat threshold than others.
The volume of fat cells your body can produce appears to reach its peak in your late teens and is influenced by your genetics.
However, research has shown that this can also be influenced by lifestyle factors such as diet and exercise.
Why are bigger fat cells bad for you?
Firstly, there’s only so much fat that an individual fat cell can store. If your body cannot produce new adipose tissue cells to store fat in times of excess energy intake, then your capacity will be limited to the current number of fat cells in your body.
Secondly, research has shown that as fat cells increase in size, they become more dysfunctional and release harmful proteins called cytokines into our bloodstream.
High levels of cytokines can increase inflammation (damage to cells) and cause insulin resistance in the muscles and adipose tissue.

Insulin resistance is when your body’s cells no longer respond to insulin, so energy from food struggles to leave the blood and enter the cells to be burnt for energy or stored for later use.
So far, our focus has been on where the body can store fat, such as under your skin as subcutaneous fat, and how this can predict your risk of developing type 2 diabetes.
It’s also clear that how your body stores fat will impact your personal fat threshold.
As we mentioned above, there will be many factors influencing how your body stores fat (i.e. whether it increases existing cell size or increases cell number), including genetics, your diet, and your levels of exercise.
Key points:
- Adipose tissue has two ways it can store excess fat:
- Hypertrophy (increase in cell size).
- Hyperplasia (increase in cell number).
- Storing excess fat through an increase in cell number (hyperplasia) is protective against developing insulin resistance and type 2 diabetes. Although genetics largely influence this, diet and exercise also impact this process to a small extent.
- Storing excess fat through an increase in cell size (hypertrophy) increases insulin resistance in the body and your risk of developing type 2 diabetes.
- Insulin resistance occurs when your body’s cells no longer respond to insulin and can’t take in energy to store or burn.
2) Insulin resistance and the adipose tissue
Insulin plays a crucial role in regulating fat and carbohydrates. When your body’s insulin levels are high, your rate of fat storage will increase, and your body will use more glucose for energy. When carbohydrate intake and insulin levels are low, your body will store less fat and use more fat for energy.
This cycle is vital for our health. Our body prefers to be in a constant cycle of efficient fuel storage and usage. Consider this energy flux, which refers to how quickly your body can move energy from the bloodstream into the cells for storage or be burnt for energy.
Suppose your body becomes insulin resistant, and fat or carbohydrate can no longer enter the muscles or the adipose tissue to be stored or burnt. In that case, it’s more likely to build up in the bloodstream, and your body will be forced to try and store it in your internal organs.
Insulin’s role is to move glucose out of the bloodstream and into the cells to either be stored as glycogen or burnt for energy. If you’re insulin resistant, the cells can do neither, and the excess glucose must be transported to other body areas to be stored as fat.
As mentioned above, your adipose tissue can also develop insulin resistance, making it difficult for fat or carbohydrate to enter the adipose tissue for storage.
If this occurs, alongside your muscle cells being insulin resistant, your body has no choice but to transport the excess energy to your internal organs.
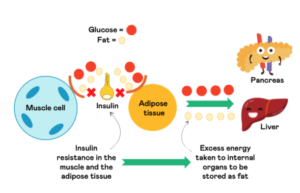
Your organs will also have a limit to how much energy they can store and will also develop insulin resistance over time. It’s at this point that excess energy, such as glucose, will build up in the bloodstream. This appears to be the basis of many chronic diseases, such as type 2 diabetes.
We primarily measure and diagnose type 2 diabetes through the haemoglobin A1c (HbA1c) test.
Haemoglobin A1c is a protein within your red blood cells that can permanently bind to sugar molecules until the red blood cell dies. When HbA1c binds to a sugar molecule, it becomes ‘glycated’ – so the blood test is the ‘glycated haemoglobin A1c’ test.
The higher your average blood sugar levels, the more haemoglobin A1c is bound to a sugar molecule. Given that red blood cells live for about 3-4 months, the HbA1c test is a great metric to give you an average of your blood sugar levels over the last 3-4 months.
It’s a sign that your body’s last lines of defence against managing excess energy have failed. Where your body, due to a variety of reasons, is no longer able to store and burn energy properly. Therefore, this energy finally builds up in the bloodstream.
Type 2 diabetes is a condition categorised by insulin resistance; likely, your level of insulin resistance in your muscles, adipose tissue, and organs is the defining characteristic of your personal fat threshold.
Key points:
- Insulin plays a vital role in the regulation of fat and carbohydrates.
- Your body wants to be in a constant cycle of storing and burning energy. For this to happen, it needs to cycle between periods of higher and lower insulin levels.
- When your body is insulin resistant, your cells no longer respond to insulin and can’t take in energy to store or burn for energy.
- Insulin resistance appears to be the underlying issue influencing the personal fat threshold.
3) Can you increase your personal fat threshold?
While our genetics will influence many elements of our personal fat threshold, it’s clear that insulin resistance is the underlying condition that can determine when you reach this point.
And while we may not have the research to support strategies to improve (or increase) your personal fat threshold, we have plenty of research on how to reduce insulin resistance and improve the function of your body’s energy systems.
In part four of this series, we’ll cover four ways to improve insulin resistance:
- A lower-carb diet based on whole foods.
- Exercise.
- Sleep.
- Stress.
Take home message
It appears that underlying every individual’s personal fat threshold is their level of insulin resistance.
Although it may be difficult to diagnose or identify an individual’s personal fat threshold, we can identify their level of insulin resistance.
Lifestyle changes such as diet, exercise, stress management, and sleep are proven strategies that reduce insulin resistance and can improve the body’s energy systems function.
In this series’s fourth and final article, we’ll discuss the critical lifestyle factors that influence your insulin resistance and how you can improve them and ensure you don’t reach your personal fat threshold.


