Understanding lupus and weight challenges
Weight gain is unfortunately common for people living with lupus.
The condition itself triggers chronic inflammation that affects how our body processes food and stores fat.
During flares, metabolism slows down significantly while the body fights the autoimmune response.
The medications used to treat lupus can also contribute to weight gain. Prednisolone, which most lupus patients take at some point, increases appetite within days of starting.
Steroids alter appetite-regulating hormones in the brain, leading to increased hunger, cravings for high-calorie foods, and reduced satiety after meals.
Research shows that lupus patients gain significant weight during steroid treatment periods.
Some gain much more, particularly if they need higher doses or longer treatment periods.
Hydroxychloroquine (Plaquenil) doesn’t usually cause weight gain directly, but it can affect blood sugar control in some people.
Methotrexate often causes nausea that leads to eating irregular meals or relying on processed foods that feel easier to tolerate.
The joint pain and fatigue associated with lupus can make regular exercise challenging.
All of this creates a cycle where lupus symptoms lead to weight gain, which then worsens lupus complications like joint stress and cardiovascular risk.
How Mounjaro works with autoimmune conditions
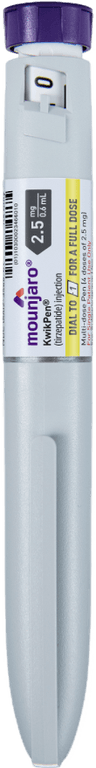
Mounjaro works by mimicking hormones called GLP-1 and GIP, which control appetite and blood sugar levels.
These hormones tell our brain when we’ve had enough to eat and help our body process glucose (sugar) more efficiently.
For lupus patients, these effects offer several potential advantages beyond weight loss.
Recent research suggests that GLP-1 medications may reduce inflammation markers, such as IL-6 and TNF-α, which are typically elevated in lupus.
Multiple studies have found that people taking GLP-1 agonists had significantly lower inflammatory markers after several months of treatment.
This anti-inflammatory effect could complement existing lupus treatments rather than interfere with them.
Think of it as an additional tool that addresses both weight and inflammation at the same time.
Mounjaro also improves insulin sensitivity, which can be particularly helpful if you’ve developed steroid-induced diabetes or pre-diabetes.
Prednisolone commonly causes insulin resistance, making blood sugar control challenging even for people without diabetes.
The hunger-lowering effect of Mounjaro can be especially valuable for lupus patients.
When steroids increase hunger, having medication that reduces those cravings can make managing our eating habits much easier.
Safety considerations and drug interactions
The safety profile for taking Mounjaro in patients with lupus looks positive based on current evidence; however, there are specific interactions and considerations to be aware of.
Direct drug interactions
Mounjaro works safely with most lupus treatments; however, some combinations require extra monitoring.
With hydroxychloroquine, both medications can potentially affect heart rhythm (specifically the QT interval on an ECG).
While this interaction is theoretical rather than proven unsafe, your doctors should know you’re taking both.
Prednisolone and Mounjaro work well together in many patients. The appetite suppression from Mounjaro can actually help manage steroid-induced hunger, making it easier to maintain a healthy diet while taking steroids.
Methotrexate doesn’t directly interact with Mounjaro, but both can occasionally affect liver function. Regular blood tests will monitor this.
Immune system considerations
One common concern is whether Mounjaro might impact immune function in individuals who already have an autoimmune condition.
Current research suggests GLP-1 medications may actually help regulate immune responses rather than suppress them.
They appear to reduce chronic low-grade inflammation while maintaining protective immune function.
However, this area requires further research, particularly in people living with autoimmune conditions.
The theoretical risk exists that any medication affecting immune signalling could influence lupus activity, though no evidence currently supports this concern.
Gastroparesis risk
Lupus can sometimes affect the nervous system, including nerves that control digestion.
This makes gastroparesis (delayed stomach emptying) slightly more likely with lupus.
Mounjaro slows gastric emptying, which could theoretically worsen existing gastroparesis.
If you have digestive symptoms like severe bloating, nausea, or feeling full after small amounts of food, discuss this with your doctor before starting Mounjaro.
Infection considerations
Some lupus patients take immunosuppressive medications that increase infection risk.
Mounjaro doesn’t suppress immune function, but any significant illness can affect both conditions.
If you develop an infection while taking Mounjaro, you may need to pause the medication temporarily while your body fights the illness, particularly if you can’t keep food down.
Coordinating care with your rheumatology team
Taking Mounjaro with lupus requires coordination between your rheumatologist and weight management provider.
Before starting Mounjaro
Your rheumatologist needs to be aware of your plans before you start. They’ll want to review your current lupus activity, recent blood test results, and medication regimen.
Ask specific questions about timing. If you’re starting a new lupus medication or changing steroid doses, it may be advisable to wait until these are stable before adding Mounjaro.
Discuss your weight loss goals realistically. Rapid weight loss can sometimes stress the body in ways that might trigger lupus flares in susceptible people.
A weight loss rate of 1-2 pounds (0.5-1 kg) per week is generally considered safe and sustainable.
Communication between teams
Your rheumatologist and weight management provider should be aware of each other’s treatment plans. This doesn’t mean they need lengthy phone calls, but key information should be shared.
Share your rheumatology blood test results with your weight management provider, particularly if they show active lupus or changing kidney function.
Let your rheumatologist know if you experience significant side effects from Mounjaro, especially if they might mimic lupus symptoms like fatigue or nausea.
Medication timing adjustments
Some patients find it helpful to adjust their medication schedule to minimise side effects.
If Mounjaro causes nausea, taking it at bedtime might help, but check that this doesn’t interfere with other medications you take at night.
Hydroxychloroquine is usually taken with food, so coordinate timing with meals while your appetite adjusts to Mounjaro.
What to monitor while taking both
Lupus patients starting Mounjaro need more frequent monitoring than people with lupus alone, but the requirements aren’t burdensome.
Blood work frequency
Most rheumatologists check the blood of lupus patients every 3-6 months when they are stable. While taking Mounjaro, you may need to undergo tests every 2-3 months initially.
Key markers to watch include kidney function (creatinine, urinalysis), liver function (ALT, AST), and lupus activity markers (complement levels, anti-DNA antibodies if you have them).
Lupus activity monitoring
Weight loss itself shouldn’t trigger lupus flares, but any significant body change can occasionally affect autoimmune conditions unpredictably.
Watch for new or worsening symptoms like joint pain, skin rashes, unusual fatigue, or fevers. These could represent normal lupus fluctuations or, rarely, reactions to new medications.
Keep a simple symptom diary if your doctor suggests it. Note energy levels, joint symptoms, and any side effects from either lupus medications or Mounjaro.
Side effect differentiation
Some symptoms could come from either lupus or Mounjaro, making it important to distinguish between them.
Nausea and fatigue can occur with both conditions. Mounjaro-related nausea usually improves within 2-4 weeks and is often related to eating. Lupus fatigue tends to be more persistent and unrelated to meals.
Digestive symptoms, such as diarrhoea, could be caused by Mounjaro, lupus affecting the gut, or medications like hydroxychloroquine. If you experience new or severe digestive symptoms, contact your healthcare team.
Losing weight sustainably
For lupus patients, gradual weight loss is generally considered safer than rapid weight loss. Aim for 1-2 pounds (0.5-1 kg) per week.
If you’re consistently losing weight faster than this, discuss adjusting your Mounjaro dose or meal planning with your healthcare provider.
Very rapid weight loss can sometimes stress the immune system.
UK-specific guidance and costs
Navigating weight management with lupus in the UK involves understanding both NHS pathways and private options.
NHS coordination
Most patients living with lupus receive care through NHS rheumatology services. Your rheumatologist can provide a letter supporting weight management if your BMI qualifies for NHS weight loss services.
Some NHS trusts offer weight management programmes specifically for people with chronic conditions like lupus. Ask your rheumatology team about local options.
NHS prescription of Mounjaro for weight loss requires meeting specific BMI criteria (usually BMI ≥35 with complications or BMI ≥30 with diabetes).
Having lupus may count as a complication supporting prescription at lower BMIs in some areas.
However, Mounjaro is currently limited on the NHS as it’s being reserved for those with the greatest clinical need (typically a BMI over 40 with multiple comorbidities).
Private treatment coordination
If you choose private weight management, ensure your NHS rheumatologist knows and supports the plan. Most are happy to coordinate care if you keep them informed.
Private Mounjaro treatment typically costs £150-250 monthly. Factor this into long-term planning, as treatment typically lasts 12-18 months, depending on your weight loss goals.
Some private providers offer specific programmes for people with chronic conditions. These may provide better coordination with your existing NHS care.
Insurance considerations
Private medical insurance occasionally covers weight management for people with obesity-related complications.
Having lupus might support coverage if weight loss could reduce steroid requirements or complications.
Check your policy details or ask your insurer directly about coverage for weight management in the context of autoimmune conditions.
Cost-benefit analysis
While private treatment involves significant costs, consider potential savings from reduced lupus complications.
Successful weight loss might reduce the need for higher steroid doses, additional medications, or joint replacement surgery.
Some patients find that losing weight improves their lupus control enough to reduce overall healthcare costs over time.
Take home message
Taking Mounjaro with lupus is generally safe and can be particularly beneficial for managing steroid-induced weight gain and potentially reducing inflammation.
Mounjaro offers a tool that addresses the hormonal and metabolic changes that make weight loss challenging for patients with lupus.
Focus on steady progress rather than rapid results, and maintain regular communication with both your rheumatologist and weight management team.
Remember that managing lupus is about more than just weight loss. Mounjaro can be part of a comprehensive approach that includes appropriate medical treatment, stress management, and gentle, consistent physical activity that supports your health in the long term.
Second Nature's Mounjaro and Wegovy programmes
Second Nature provides Mounjaro or Wegovy as part of our Mounjaro and Wegovy weight-loss programmes.
Why choose Second Nature over other medication providers, assuming you're eligible?
Because peace of mind matters.
We've had the privilege of working with the NHS for over eight years, helping people across the UK take meaningful steps toward a healthier, happier life.
Our programmes are designed to meet people where they are, whether that means support with weight loss through compassionate one-to-one health coaching, or access to the latest weight-loss medications (like Mounjaro and Wegovy) delivered alongside expert care from a multidisciplinary team of doctors, psychologists, dietitians, and personal trainers.
At the heart of everything we do is a simple belief: real, lasting change comes from building better habits, not relying on quick fixes. We're here to support that change every step of the way.
With over a decade of experience, thousands of lives changed, and a long-standing record of delivering programmes used by the NHS, we believe we're the UK's most trusted weight-loss programme.
We hope to offer you something invaluable: peace of mind, and the support you need to take that first step.