Jump to: What is the DASH diet? | Is the DASH diet healthy? | The DASH diet can improve blood pressure | The DASH diet may have moderate effects on weight management | The DASH diet doesn’t come without downsides | Take home message
Is the DASH diet healthy? Theoretically, yes, but with some downsides
From a nutritional perspective, the DASH diet can be viewed as a healthy diet as it prioritises the consumption of whole foods while minimising the intake of ultra-processed foods, particularly those rich in sugar.
It’s been shown to impact blood pressure in individuals living with hypertension positively. Research also suggests it can have moderate effects on weight loss and markers of type-2 diabetes, such as insulin resistance.
However, research has focused on individuals with pre-existing hypertension (or those at risk of hypertension), and it’s unclear whether the diet would have any added beneficial effects on otherwise healthy individuals.
There’s also a lack of long-term data to determine how sustainable it is in practice and whether the restriction of dietary fat and sodium (salt) would have any unintended consequences in the long term.
The focus on restricting fat from whole foods, such as dairy, and consuming more starchy carbohydrates may increase the risk of developing insulin resistance, particularly if individuals opt for refined carbohydrates such as white bread, rice, and cereals.
The DASH diet also recommends consuming very low levels of salt (less than 2g per day). This is despite research showing that salt intakes below 2g per day are associated with a higher risk of all-cause mortality than individuals eating moderate to higher intakes.
The DASH (Dietary Approaches to Stop Hypertension) diet was first introduced in 1997 and is promoted by the US National Institute of Health’s Heart, Lung, and Blood Institute (NHBLI).
It’s been heavily researched, with many public health organisations advocating it for individuals living with hypertension.
What is the DASH diet?
It’s a low-fat diet with specific recommendations to lower saturated fat, salt, and cholesterol and was designed by the NHBLI to target individuals living with high blood pressure.
The DASH diet encourages the consumption of:
- Whole grains
- Starchy carbohydrates
- Fruits and vegetables
- Low-fat dairy
- Lean meats
- Fish and seafood
- Small amounts of fat from plant-based sources such as avocado and olive oil
The DASH diet discourages the consumption of:
- Red and processed meats
- Sweets and other high sugar, ultra-processed foods
- Added salt
- Foods high in saturated fat, such as butter and cream
At Second Nature, we don’t provide strict guidelines on what to eat. Our nutritional guidelines are designed to be flexible and personalised to the individual while allowing you the freedom to experiment with what works best for you.
You can take our health quiz here if you want to give us a go.
Otherwise, keep reading if you’d like to read the science behind the pros and cons of the DASH diet. You’ll find three sections reviewing different lines of evidence with a brief conclusion at the end.
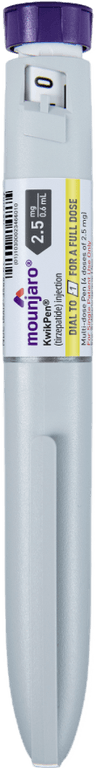
Medication-assisted weight loss with a future focus
Start with Wegovy or Mounjaro, transition to habit-based health with our support

1) The DASH diet can improve blood pressure
Blood pressure measures how much pressure is placed on the walls of the vessels in your circulatory system, such as your arteries and veins.
It’s measured in units of millimetres of mercury (mmHg), and there are two ways that blood pressure is displayed:
Systolic (normal <120mmhg): the pressure when the heart beats
Diastolic (normal <80mmhg): the pressure when the heart relaxes
High blood pressure is associated with the development of heart disease, and maintaining healthy levels is a strong indicator of your health.
A randomised controlled feeding trial compared the effect of the DASH diet, a standard American diet with added fruit and vegetables, and a standard American diet without added fruits and vegetables, on blood pressure in over 400 participants with hypertension.
The DASH diet reduced both systolic by 5.5mmHg and diastolic by 3mmHg more than the standard American diet, which saw no change in blood pressure from baseline.
Surprisingly, the DASH diet saw no changes in salt intake from baseline but an increase in potassium (which has a vital role in blood pressure management) alongside the improvement in the overall diet.
Further trials investigating the impact of the DASH diet with varying levels of salt intake have also supported this finding. This suggests that you can improve your blood pressure without reducing your salt intake by improving your overall diet and potassium intake.
This is further illustrated by a meta-analysis (a type of study that compares the results of many different trials) that compared the effects of four diets based on whole food consumption on blood pressure reduction. It showed that all of the dietary patterns have a positive impact on blood pressure.
Key points:
- Many human trials have shown that the DASH diet can positively impact blood pressure
- These improvements can’t be explained by salt intake and are more likely related to the improvement in overall diet changes and increased potassium intake
- Meta-analysis of other dietary patterns based on whole foods has also shown improvements in blood pressure
- While the DASH diet clearly shows benefits, it’s not the only approach people can choose to improve their blood pressure
2) The DASH diet may have moderate effects on weight management
Considering the association between obesity and chronic diseases such as type-2 diabetes and heart disease, achieving a healthy weight is an important indicator of our overall health.
A randomised controlled trial in free-living individuals was conducted to investigate the impact of two calorie-restricted diets—a DASH diet and a control diet that contained fewer fruits and vegetables and higher amounts of sugar.
The study showed modest reductions in weight in both groups, with the DASH diet participants losing an average of 3.8kg and the control group losing 2.6kg after eight weeks.
Unfortunately, no longer-term studies have been conducted looking at the effects of the DASH diet on weight loss. It’s therefore difficult to determine how sustainable it would be for people in real-world conditions outside of a research environment.
Recent research has also shown that restricting dietary fat during weight loss may change dopamine (a hormone involved in motivation and reward) signalling in the brain. This encouraged the consumption of ultra-processed foods rich in refined carbohydrates, added fat, and sugar.
This suggests that the focus on restricting fat in the DASH diet may limit its effectiveness as a weight loss solution in the long term.
Key points:
- The DASH diet may have moderate effects on weight loss
- Due to a lack of long-term data, and its focus on restricting dietary fat, it’s unclear whether the DASH diet is a sustainable approach to support weight management
3) The DASH diet doesn’t come without downsides
Restricting fat isn’t sustainable for most people
One of the recommendations on the DASH diet is to reduce your dietary fat intake. This coincides with many global public health guidelines recommending a low-fat diet for overall health.
Despite these recommendations, many human trials have shown the positive effects of consuming higher amounts of fat to support our health, most notably to aid weight loss.
A recent randomised controlled trial compared a lower-fat DASH diet to a higher-fat DASH diet to determine their effects on weight loss outcomes and other risk factors for cardiovascular disease such as very-low-density lipoprotein (VLDL) and triglycerides.
The study showed that both the lower-fat and higher-fat DASH diets improved blood pressure to a similar degree.
But interestingly, the higher-fat DASH diet saw more significant reductions in VLDL and triglycerides – suggesting a greater improvement in overall risk for cardiovascular disease.
Before this trial, the sole focus of the DASH diet on blood pressure has likely prevented further analysis of other markers that also influence our health.
When deciding whether a diet is healthy, we must look at the whole picture rather than isolating one aspect.
For example, suppose we were to isolate blood sugar as the only meaningful measure of our health.
In that case, we might recommend a diet that includes only butter, as it would almost guarantee perfect blood sugar levels. But over the long term, we’d likely develop micronutrient deficiencies that would negatively affect our health.
Very low salt intake may be harmful to our health
Extensive observational studies – using estimated intakes based on food availability data – have suggested that low-salt intakes are associated with the lowest blood pressure and the lowest rates of cardiovascular disease.
Unfortunately, intake estimates aren’t the most reliable way to investigate the cause and effect of one nutrient on our health.
Alongside this, these studies failed to identify where the salt came from in the diet.
Therefore, it’s possible these individuals were consuming high levels of salt due to a diet high in ultra-processed foods rather than a healthy diet that also included high levels of salt.
A more accurate measure of salt intake is to measure the amount of sodium we excrete out of our urine, as this highly correlates with the amount we consume in our diets. We can then determine what impact this has on our health.
A study on over 100,000 individuals in 17 countries investigated the impact of salt, measured by urinary sodium levels, on all-cause mortality and the risk of experiencing a cardiovascular event, such as a heart attack or a stroke.
The study showed that a very high salt intake of more than 6g per day was associated with a slightly higher risk of cardiovascular disease and all-cause mortality compared to moderate amounts between 3-6g per day.
Surprisingly, the highest risk was seen in low salt intakes of less than 2g per day. This suggests that very low salt intakes below 2g per day may be detrimental to our health, while moderate intakes are beneficial.
Key points
- The DASH diet recommends restricting dietary fat, but research has shown that higher-fat intakes can positively impact our health, particularly in supporting weight loss.
- Lower-fat DASH diets may be difficult to sustain in the long term.
- The DASH diet recommends consuming very low levels of salt (less than 2g per day), but recent research suggests that very low salt intake could be more harmful to our health than moderate to higher intakes.
Take home message
The DASH diet has positively affected blood pressure in many human trials. Still, advocates for this approach might be missing the bigger picture by isolating blood pressure and failing to reflect on the overall impact of the diet on our health.
Like any diet, the issue often comes down to sustainability, and the DASH diet is no different. It may be very effective at reducing blood pressure in the short term, but its long-term effects on human health are unclear.