Jump to: Three ways to beat the winter blues | Get outdoors | What to eat to beat the winter blues | Light therapy | Take home message
The winter blues, or seasonal affective disorder (SAD), affects up to 2 million people in the UK and 10-20 million in the US. The severity of the condition appears on a spectrum, with some people experiencing milder symptoms than others.
The actual causes of SAD are not fully understood and are likely to be multifactorial. Still, research suggests that people living with SAD have dysregulated melatonin release and an altered response to light compared to those without SAD. Melatonin is a neurotransmitter that helps to regulate our sleep/wake cycle.
Fortunately, there are three evidence-based ways to manage the condition in the winter and ensure you’re feeling more optimistic as we head into the darker months of the year.
Three ways to beat the winter blues
- Get outdoors: The days may be shorter and the weather harsher, but good evidence suggests getting outside while it’s still bright during the day, particularly accessing nature and green space, boosts mood.
- Eat a diet based on whole foods: The gut-brain connection plays a role in managing our mental and physical health. Strong evidence suggests that diets based on whole foods can reduce depression and improve mental health.
- Light therapy: Light therapy trials have shown that symptoms of SAD improve and melatonin secretion returns to more normal levels. Making a simple, cost-effective solution to managing SAD over the winter.
At Second Nature, you’re supported by a registered dietitian or nutritionist who can guide you on implementing healthier lifestyle habits that can improve your health and mood year-round.
You can join over 150,000 members like Becky, who’ve joined Second Nature and seen their energy levels and mood improve. All you’d need to do to start is click here to take our health quiz.
Otherwise, keep reading as we dig deeper into the three ways you can beat the winter blues.
1) Get outdoors
Many of us inherently know the benefits of getting outside. You generally feel better if you spend more time outdoors. Fortunately, evidence suggests this isn’t just an old wives tale but an evidence-based approach to improving your mood, lowering your stress levels, and helping you beat the winter blues.
A review of 43 observational studies investigating the impact of spending time outdoors found strong associations between outdoor activities – particularly those with green space – such as gardening, nature viewing, and exercising with lower self-reported stress, blood cortisol levels (our stress hormone), and physical health markers such as blood pressure.
The relationship between the outdoors and cortisol is an important one. Cortisol seems to work in partnership with melatonin to help regulate our sleep-wake cycle. If cortisol levels are too high, this can prevent melatonin from having its desired effects in supporting the body to wind down in the evening.
Interestingly, the sun might be playing a role in this relationship. A small study recruited 9 participants who all completed the following exposures:
- Natural sunlight
- Artificial UV radiation
- Spending time in darkness
They measured hair cortisol (a reliable marker of long term cortisol levels) in the participants before and after the interventions. They found that natural sunlight and artificial UV exposure similarly lowered hair cortisol (54% & 75%). At the same time, the darkness intervention experienced no changes.
Similarly, research has shown that alongside this change in cortisol levels, accessing the outdoors can lead to clinical improvements in the symptoms associated with SAD and depression. A study randomised participants diagnosed with SAD into two groups:
- Natural light: A one-hour morning walk
- Artificial light: 30-minutes of a low-dose light therapy treatment
The study used a validated assessment tool (Hamilton Depression Rating Scale) to evaluate the participant’s depression ratings. The artificial light saw improvements in some ratings of depression, and 25% achieved remission, where they were considered to no longer be living with depression.
Contrastingly, the natural light group saw improvements in all ratings of depression, and 50% of the participants achieved remission and were considered to no longer be living with depression.
This research suggests that artificial and natural light can help reduce cortisol levels and improve SAD and depression. But considering the other benefits of getting outdoors, such as physical exercise and social interaction, ensuring you’re spending as much time as possible outside is likely to lead to multiple health benefits beyond SAD.
Here are some tips for getting outdoors this winter:
- Have a walk or exercise outdoors in the morning or lunchtime; try to involve the whole family or invite friends for accountability.
- Join a local walking group or sports club.
- Get a dog.
Key points:
- Observational research suggests that people who spend more time outdoors and in natural environments report lower stress levels, lower cortisol levels, and better physical health.
- Cortisol plays a key role in regulating our sleep-wake cycle in partnership with Melatonin. If cortisol levels are too high, this can disrupt this relationship.
- Natural light exposure has been shown to lower cortisol levels and reduce symptoms of SAD and clinical depression in human trials.
2) What to eat to beat the winter blues
The gut-brain connection was a relatively untapped area of research until recently. We now know that the gut communicates directly with the brain via neurotransmitters and hormones produced and released by the gut. This relationship explains how our diet can impact our mood and mental health.
Unfortunately, there’s very little research explicitly measuring the effects of diet on SAD. A meta-analysis investigating the connection between diet and SAD found only three trials using diet as an intervention for SAD, and there was no conclusive evidence of an effect.
This was likely due to the trials only comparing high-carbohydrate VS high-protein diets while not considering overall diet quality. Future trials on people living with SAD should focus on the impact of an overall diet based on whole foods that incorporates a healthy balance of all food groups.
Interestingly, the study did analyse four studies showing an association between those following a vegetarian diet and higher rates of depression compared to non-vegetarians. A possible reason for this could be the inadequate intake of an essential amino acid known as tryptophan which is readily found in animal-based proteins.
Tryptophan is required for the production of serotonin in the brain, a vital neurotransmitter implicated in developing mental health conditions like depression.
If you’re a vegan or a vegetarian, it’s recommended to consume foods like dairy (vegetarian), oats, nuts and seeds, and soy-based products like tofu and soy milk to ensure you’re consuming enough tryptophan.
While there’s not a lot of human research on diet and SAD, we can draw on other studies looking at the impact of diet on other mental health conditions, such as depression.
One study known as the SMILES trial examined whether diet could improve depressive symptoms in 166 individuals diagnosed with clinical depression undergoing treatment (either medication, therapy, or both).
Half the participants were instructed to follow a Mediterranean-style diet (lots of vegetables, fish, whole grains, and fat from extra virgin olive oil and whole meat). At the same time, the other half received social support sessions in line with the traditional treatment of depression.
The dietary intervention group experienced a more substantial reduction in depressive symptoms over the three months. In addition, significantly more participants in the diet group met the criteria for remission of clinical depression.
Correspondingly, another trial investigating the impact of the Mediterranean diet – supplemented with additional fish oil – found significant improvements in depression and mental health after six months.
This doesn’t mean we all need to eat a Mediterranean diet, but we can take inspiration from the foundations of the diet, which are based on an intake of whole foods such as vegetables, fish, extra virgin olive oil, whole grains, and meat.
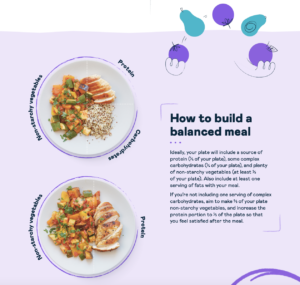
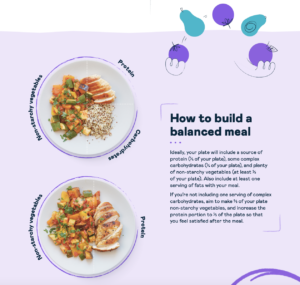
Click here if you’d like a free NHS-trusted meal plan from Second Nature. Also, feel free to download this image outlining how to build a balanced meal.
Key points:
- The gut-brain connection explains the relationship between our diet and mental health.
- No conclusive evidence suggests that diet plays a role in reducing symptoms of SAD, but this is likely due to the design of the studies as opposed to an absence of a possible effect.
- Vegetarians may be at a higher risk of depression compared to non-vegetarians. An inadequate intake of tryptophan might explain this relationship.
- Two large randomized controlled trials have shown that a Mediterranean diet based on whole foods can positively affect depression and mental health.
3) Light therapy
While it might not provide all of the benefits of accessing the outdoors, we’ve seen above that light therapy can be an effective treatment for reducing SAD symptoms. Light therapy also supports individuals living with SAD who might have difficulties accessing the outdoors, such as those working night shifts or living with physical disabilities.
A study recruited 50 adults with mild and severe SAD and randomised them to either a three-week light therapy treatment or no treatment (control). The study showed that the light therapy intervention significantly reduced depression scores, and 64% had normal depression scores after the treatment.
Similarly, a recent trial investigated the impact of bright white light therapy and dim red light therapy on the depression scores of participants living with SAD. The study showed that both interventions saw reductions in depression scores of over 40%.
Interestingly, research has shown that individuals living with SAD appear to have an abnormal function in their retina (the light-sensitive part of our eye) during the winter, which normalises in the summer and may also be responsive to light therapy treatment. This might explain the difference in melatonin secretion observed in individuals living with SAD.
The study showed that after four weeks of a light therapy intervention, the retina’s function returned to normal. Participants living with SAD had similar light sensitivity as those who didn’t have SAD.
You can find some recommended light therapy lamps here.
Key points:
- Light therapy provides a cost-effective and practical solution to manage SAD and improve the symptoms associated with it.
- Human clinical trials have shown promising results in using light therapy to treat SAD and clinical depression.
- Light therapy appears to work by normalising the retina’s function, which may help the body’s melatonin production.
Take home message
The winter blues, or SAD can be a severe clinical disorder that has a significant impact on your quality of life. It can also come in milder forms where you might not have a clinical diagnosis, but you still feel the effect of the winter months on your general mood and health.
While you can’t control your susceptibility to developing SAD, there are practical changes you can make to your lifestyle that are simple in practice but may have a significant impact on your health and well-being.
Why not give one of them a go this week and see how your mood changes?