What is a tier 3 weight management service?
Tier 3 weight management services represent the NHS’s most intensive obesity treatment programmes, designed for people with complex health needs who haven’t succeeded with conventional approaches.
These specialist services go far beyond simply prescribing medication, offering a complete multidisciplinary approach to weight loss.
The tier 3 team typically includes:
- Consultant endocrinologists or bariatric physicians
- Specialist dietitians trained in obesity management
- Clinical psychologists addressing eating behaviours
- Physiotherapists for safe exercise programmes
- Specialist nurses for ongoing support
Programmes run for 12-18 months and include regular appointments, group sessions, and comprehensive lifestyle interventions alongside any prescribed medications.
The service aims to achieve sustainable weight loss of at least 10-15% of starting weight, with many participants losing significantly more when combining support with medications like Saxenda3.
However, availability varies drastically across the UK, with some areas having well-funded services while others have minimal provision.
According to NHS England data, only about 3% of eligible adults can access tier 3 services due to capacity constraints2.
NHS eligibility criteria for Saxenda
Meeting the eligibility criteria for NHS-funded Saxenda involves more than just having a high BMI, as services must prioritise those with the greatest clinical need.
Primary eligibility requirements:
- BMI ≥40 kg/m² without other conditions, OR
- BMI ≥35 kg/m² with one or more obesity-related conditions such as:
- Type 2 diabetes
- High blood pressure requiring medication
- Sleep apnoea
- Osteoarthritis affecting mobility
- Polycystic ovary syndrome (PCOS)
- Age 18 or over (some services accept 16+)
- Documented evidence of previous weight loss attempts
- Commitment to 12-18 month programme
You may be excluded if you:
- Are pregnant, breastfeeding, or planning pregnancy
- Have active eating disorders
- Have severe mental health conditions affecting engagement
- Cannot attend regular appointments
- Have medical contraindications to Saxenda
Some areas apply additional local criteria, such as requiring completion of tier 2 services first or living within specific postcodes.
The assessment team considers your whole health picture, not just weight, including psychological readiness for change and support systems.
| Criteria |
Standard requirement |
Additional notes |
| BMI threshold |
≥35 with conditions or ≥40 |
Some areas use ≥30 for diabetes |
| Previous attempts |
6-12 months documented |
Must include lifestyle changes |
| Waiting time |
3-12 months typically |
Varies significantly by region |
| Programme length |
12-18 months |
Includes regular reviews |
Getting referred for Saxenda on the NHS
The referral process for NHS Saxenda begins with your GP, who acts as the gatekeeper to specialist services and must believe you meet the criteria.
Step 1: Prepare for your GP appointment
Document your weight history, including all previous diet attempts, commercial programmes tried, and any weight-related health issues you’re experiencing.
Bring a weight diary showing at least 6 months of attempted weight loss through diet and exercise.
List all obesity-related symptoms affecting your quality of life, from joint pain to sleep problems.
Step 2: The GP assessment
Your GP will calculate your BMI, review your medical history, and assess whether you meet tier 3 criteria.
They may order blood tests to check for diabetes, thyroid function, and other metabolic conditions.
Some GPs might suggest trying their practice’s weight management support first if you haven’t already.
Step 3: Making the referral
If approved, your GP will complete a detailed referral form that includes your medical history, current medications, and the reasons for referral.
The referral is sent to your local Tier 3 service, although you may wait several weeks for an acknowledgement.
You should receive a letter confirming your referral and estimated waiting time.
What if your GP refuses a referral?
Request a clear explanation of why you don’t meet the criteria and what you need to do to qualify.
Consider seeking a second opinion from another GP in your practice.
You can formally complain through the practice complaints procedure if you believe you meet NHS England criteria.
Some people choose to self-fund private assessments to demonstrate their commitment, then return to their GP.
The tier 3 assessment process
Once accepted for assessment, you’ll undergo a comprehensive evaluation that goes far beyond a simple weight check, typically involving multiple appointments over several weeks.
Initial medical assessment (2-3 hours)
A consultant reviews your complete medical history, including childhood weight patterns, family history, and all previous weight loss attempts.
Physical examination includes detailed measurements, blood pressure, and assessment for obesity-related conditions.
You’ll discuss your eating patterns, trigger foods, and relationship with food in detail.
Blood tests check for hormonal imbalances, diabetes, liver function, and vitamin deficiencies.
Psychological evaluation (1-2 hours)
A clinical psychologist explores your emotional relationship with food and any underlying mental health concerns.
They assess for eating disorders, depression, anxiety, and readiness for change.
You might complete questionnaires about eating behaviours, mood, and quality of life.
This isn’t about judging you, but ensuring you get appropriate psychological support.
Dietetic assessment (1 hour)
A specialist dietitian analyses your current diet through food diaries and discusses realistic changes.
They identify nutritional deficiencies and create initial meal planning strategies.
Education covers portion sizes, reading food labels, and managing social eating situations.
Physical activity assessment (45 minutes)
A physiotherapist evaluates your mobility, joint problems, and exercise capacity.
They design a safe, gradual exercise programme considering your physical limitations.
This might start with just 5-10 minutes of gentle movement daily.
Multidisciplinary team (MDT) meeting
After assessments, the team meets to discuss your case and decide on treatment recommendations.
They consider whether Saxenda is appropriate or if other interventions should be tried first.
You’ll receive a detailed treatment plan including medication, dietary changes, exercise goals, and psychological support.
If approved for Saxenda, you’ll start with careful monitoring and regular follow-ups every 2-4 weeks initially.
Alternative weight-loss medications to Saxenda
While Saxenda was groundbreaking when launched, newer GLP-1 medications now offer superior weight loss results with better tolerability and convenient weekly dosing4.
Wegovy (semaglutide)
Wegovy represents the next generation of GLP-1 medications, showing average weight loss of 15-17% compared to Saxenda’s 5-7%5.
The weekly injection means better compliance than Saxenda’s daily injections.
Side effects are generally milder, with less nausea reported in clinical trials.
NHS availability is currently limited but expanding, with some areas now offering it through tier 3 services.
Private prescription costs range from £150-250 monthly.
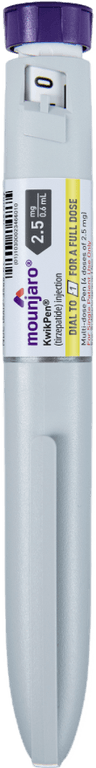
Mounjaro (tirzepatide)
Mounjaro combines GLP-1 and GIP hormone effects, achieving the highest weight loss of any approved medication at 20-25% average reduction6.
Weekly injections with a simple dose escalation schedule.
Particularly effective for people with type 2 diabetes, often allowing medication reduction.
Currently available privately in the UK at £200-400 per month, depending on the dose.
It’s available on the NHS following NICE approval7, but availability is very limited.
Orlistat (Xenical/Alli)
The only medication available without a specialist referral works by blocking fat absorption in the gut.
Much more modest weight loss of 3-5% on average.
Unpleasant side effects when eating meals high in fat.
Available on NHS prescription from GPs or over the counter.
Costs around £20-£50 per month.
| Medication |
Average Weight Loss |
Dosing |
Monthly Cost (Private) |
| Saxenda |
5-7% |
Daily injection |
£150-300 |
| Wegovy |
15-17% |
Weekly injection |
£150-250 |
| Mounjaro |
20-25% |
Weekly injection |
£200-400 |
| Orlistat |
3-5% |
Three times daily |
£20-50 |
Second Nature offers both Wegovy and Mounjaro as part of comprehensive programmes including dietitian support, habit change coaching, and long-term maintenance strategies.
Research shows that combining medication with behavioural support doubles the chances of maintaining weight loss after stopping treatment5.
Private prescription options for Saxenda
With NHS waiting lists extending beyond 12 months in many areas, private prescriptions offer immediate access to Saxenda, though costs and quality vary significantly between providers.
Online weight management clinics
Reputable online providers offer consultant assessments, prescriptions, and varying levels of support.
Costs typically include consultation fees (£50-150) plus medication (£150-300 monthly).
Look for CQC-registered providers with GMC-registered doctors.
Be wary of sites offering prescriptions without a proper medical assessment.
The best services include ongoing support from dietitians or nutritionists.
Private weight loss clinics
Physical clinics provide face-to-face assessments and monitoring.
Often more expensive (£200-400 monthly) but includes regular check-ups.
Some offer comprehensive programmes similar to NHS tier 3 services.
May have payment plans or package deals for longer treatment.
Useful if you prefer in-person support or have complex health needs.
Private endocrinologists
Specialist consultants offer the most thorough assessment and monitoring.
Initial consultations cost £200-400 with follow-ups at £100-200.
They can manage complex cases and adjust medications optimally.
Often have shorter waiting times than NHS services.
May coordinate with your NHS GP for some monitoring.
What to consider with private prescriptions:
- No guarantee of long-term results without lifestyle changes
- Costs continue monthly for as long as you take medication
- The quality of support varies dramatically between providers
- Some providers prioritise sales over patient safety
- Check what happens when you want to stop treatment
Without proper support, most people regain weight after stopping medication, making the total investment potentially thousands of pounds for temporary results.
Frequently asked questions
How long does it take to get Saxenda on the NHS?
From GP referral to starting medication typically takes 3-12 months, depending on your area’s waiting lists and assessment process. Some regions report waits exceeding 18 months due to high demand and limited capacity in tier 3 services.
Can my GP prescribe Saxenda directly?
No, GPs cannot prescribe Saxenda for weight loss under current NHS guidelines. They must refer you to a specialist tier 3 weight management service where consultants can prescribe it as part of a comprehensive programme. Some GPs may prescribe it privately, but this is uncommon.
What happens if I’m refused NHS funding for Saxenda?
If refused, request a written explanation of the decision and what you need to do to qualify. You can appeal through your local Clinical Commissioning Group’s appeals process. Alternatively, consider whether newer medications, such as Wegovy, might be available, or explore private options if financially feasible.
How much weight will I lose with Saxenda?
Clinical trials show average weight loss of 5-7% of starting weight over 12 months when combined with diet and exercise4. However, newer medications like Wegovy (15-17%) and Mounjaro (20-25%) achieve significantly better results, which is why many specialists now prefer these options.
Does Saxenda work better than Wegovy or Mounjaro?
No, clinical evidence clearly shows Wegovy and Mounjaro achieve 2-3 times more weight loss than Saxenda5,6. They also require less frequent injections (weekly vs daily) and many patients report fewer side effects. Saxenda remains useful for some patients but is no longer considered the gold standard.
What are the main side effects of Saxenda?
Common side effects include nausea (40% of users), diarrhoea (20%), constipation (20%), and injection site reactions. Most side effects improve after 4-6 weeks as your body adjusts. Serious side effects are rare but include pancreatitis and gallbladder problems requiring immediate medical attention.
Can I stay on Saxenda long-term through the NHS?
NHS funding typically covers 12-18 months of treatment within tier 3 services. Continued prescribing depends on achieving at least 5% weight loss by 3 months and maintaining progress. Long-term NHS prescriptions are rare, with most patients expected to maintain weight through lifestyle changes alone.
Is it worth paying privately for Saxenda instead of waiting?
This depends on your financial situation and urgency. Private treatment costs £150-300 monthly indefinitely, potentially totalling thousands of pounds.
Consider whether newer medications might offer better value, and ensure any private provider includes proper support for sustainable lifestyle changes alongside medication.
Take home message
Getting Saxenda on the NHS requires meeting strict eligibility criteria through tier 3 weight management services.
While the comprehensive support these services provide is excellent, waiting times of 6-12 months or more mean many people need to consider alternatives.
The landscape of weight loss medications has evolved significantly, with newer options like Wegovy and Mounjaro offering superior results to Saxenda’s 5-7% average weight loss.
Whether you pursue NHS funding or private prescriptions, remember that medication alone rarely leads to lasting weight loss without addressing underlying habits and behaviours.
The decision between waiting for NHS treatment or investing in private care is deeply personal, depending on your health urgency, financial situation, and previous weight loss experiences.
Whatever path you choose, ensure you’re getting comprehensive support, not just medication, as this combination offers the best chance of achieving and maintaining a healthier weight for life.
Second Nature's Mounjaro and Wegovy programmes
Second Nature provides Mounjaro or Wegovy as part of our Mounjaro and Wegovy weight-loss programmes.
Why choose Second Nature over other medication providers, assuming you're eligible?
Because peace of mind matters.
We've had the privilege of working with the NHS for over eight years, helping people across the UK take meaningful steps toward a healthier, happier life.
Our programmes are designed to meet people where they are, whether that means support with weight loss through compassionate one-to-one health coaching, or access to the latest weight-loss medications (like Mounjaro and Wegovy) delivered alongside expert care from a multidisciplinary team of doctors, psychologists, dietitians, and personal trainers.
At the heart of everything we do is a simple belief: real, lasting change comes from building better habits, not relying on quick fixes. We're here to support that change every step of the way.
With over a decade of experience, thousands of lives changed, and a long-standing record of delivering programmes used by the NHS, we believe we're the UK's most trusted weight-loss programme.
We hope to offer you something invaluable: peace of mind, and the support you need to take that first step.
References
-
- National Institute for Health and Care Excellence. (2020). Liraglutide for managing overweight and obesity (TA664)
- Mid and South Essex Integrated Care System. (2024). Updates to Tier 3 Eligibility Criteria
- Hazlehurst, J.M., et al. (2020). Developing Integrated Clinical Pathways for the Management of Clinically Severe Adult Obesity: a Critique of NHS England Policy. Current Obesity Reports, 5(3), 320-326.
- Pi-Sunyer, X., et al. (2015). A Randomized, Controlled Trial of 3.0 mg of Liraglutide in Weight Management. New England Journal of Medicine, 373(1), 11-22.
- Wilding, J.P.H., et al. (2021). Once-Weekly Semaglutide in Adults with Overweight or Obesity. New England Journal of Medicine, 384(11), 989-1002.
- Jastreboff, A.M., et al. (2022). Tirzepatide Once Weekly for the Treatment of Obesity. New England Journal of Medicine, 387(3), 205-216.
- National Institute for Health and Care Excellence. (2023). Tirzepatide for treating type 2 diabetes (TA924)